Insulin-like growth factor 1
Insulin-like growth factor 1 (IGF-1), also called somatomedin C, is a hormone similar in molecular structure to insulin which plays an important role in childhood growth, and has anabolic effects in adults.[5] In the 1950s IGF-1 was called "sulfation factor" because it stimulated sulfation of cartilage in vitro,[6] and in the 1970s due to its effects it was termed "nonsuppressible insulin-like activity" (NSILA).[7]
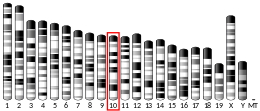
IGF-1 is a protein that in humans is encoded by the IGF1 gene.[8][9] IGF-1 consists of 70 amino acids in a single chain with three intramolecular disulfide bridges. IGF-1 has a molecular weight of 7,649 daltons.[10] In dogs, an ancient mutation in IGF1 is the primary cause of the toy phenotype.[11]
IGF-1 is produced primarily by the liver. Production is stimulated by growth hormone (GH). Most of IGF-1 is bound to one of 6 binding proteins (IGF-BP). IGFBP-1 is regulated by insulin. IGF-1 is produced throughout life; the highest rates of IGF-1 production occur during the pubertal growth spurt.[12] The lowest levels occur in infancy and old age.[13][14]
Low IGF-1 levels are associated with cardiovascular disease, while high IGF-1 levels are associated with cancer. Mid-range IGF-1 levels are associated with the lowest mortality.
A synthetic analog of IGF-1, mecasermin, is used for the treatment of growth failure in children with severe IGF-1 deficiency.[15] Cyclic glycine-proline (cGP) is a metabolite of hormone insulin-like growth factor-1 (IGF-1). It has a cyclic structure, lipophilic nature, and is enzymatically stable which makes it a more favourable candidate for manipulating the binding-release process between IGF-1 and its binding protein, thereby normalising IGF-1 function.[16]
Synthesis and circulation
[edit]The polypeptide hormone IGF-1 is synthesized primarily in the liver upon stimulation by growth hormone (GH). It is a key mediator of anabolic activities in numerous tissues and cells, such as growth hormone-stimulated growth, metabolism and protein translation.[17] Due to its participation in the GH-IGF-1 axis it contributes among other things to the maintenance of muscle strength, muscle mass, development of the skeleton and is a key factor in brain, eye and lung development during fetal development.[18]
Studies have shown the importance of the GH-IGF-1 axis in directing development and growth, where mice with a IGF-1 deficiency had a reduced body- and tissue mass. Mice with an excessive expression of IGF-1 had an increased mass.[19]
The levels of IGF-1 in the body vary throughout life, depending on age, where peaks of the hormone is generally observed during puberty and the postnatal period. After puberty, when entering the third decade of life, there is a rapid decrease in IGF-1 levels due to the actions of GH. Between the third and eight decade of life, the IGF-1 levels decrease gradually, but unrelated to functional decline.[18] However, protein intake is proven to increase IGF-1 levels.[20]

Mechanism of action
[edit]IGF-1 is a primary mediator of the effects of growth hormone (GH). Growth hormone is made in the anterior pituitary gland, released into the bloodstream, and then stimulates the liver to produce IGF-1. IGF-1 then stimulates systemic body growth, and has growth-promoting effects on almost every cell in the body, especially skeletal muscle, cartilage, bone, liver, kidney, nerve, skin, hematopoietic, and lung cells. In addition to the insulin-like effects[further explanation needed], IGF-1 can also regulate cellular DNA synthesis.[21]
IGF-1 binds to at least two cell surface receptor tyrosine kinases: the IGF-1 receptor (IGF1R), and the insulin receptor. Its primary action is mediated by binding to its specific receptor, IGF1R, which is present on the surface of many cell types in many tissues[further explanation needed]. Binding to the IGF1R initiates intracellular signaling. IGF-1 is one of the most potent natural activators of the Akt signaling pathway, a stimulator of cell growth and proliferation, and a potent inhibitor of programmed cell death.[22][23] The IGF-1 receptor and insulin receptor are two closely related members of a transmembrane tetrameric tyrosine kinase receptor family. They control vital brain functions, such as survival, growth, energy metabolism, longevity, neuroprotection and neuroregeneration.[24]
Metabolic effects
[edit]As a major growth factor, IGF-1 is responsible for stimulating growth of all cell types, and causing significant metabolic effects.[25] One important metabolic effect of IGF-1 is signaling cells that sufficient nutrients are available for them to undergo hypertrophy and cell division.[26] Its effects also include inhibiting cell apoptosis and increasing the production of cellular proteins.[26] IGF-1 receptors are ubiquitous, which allows for metabolic changes caused by IGF-1 to occur in all cell types.[25] IGF-1's metabolic effects are far-reaching and can coordinate protein, carbohydrate, and fat metabolism in a variety of different cell types.[25] The regulation of IGF-1's metabolic effects on target tissues is also coordinated with other hormones such as growth hormone and insulin.[27]
The IGF system
[edit]IGF-1 is part of the insulin-like growth factor (IGF) system.[28] This system consists of three ligands (insulin, IGF-1 and IGF-2), two tyrosine kinase receptors (insulin receptor and IGF-1R receptor) and six ligand binding proteins (IGFBP 1–6).[28] Together they play an essential role in proliferation, survival, regulation of cell growth and affect almost every organ system in the body.[29]
Similarly to IGF-1, IGF-2 is mainly produced in the liver and after it is released into circulation, it stimulates growth and cell proliferation. IGF-2 is thought to be a fetal growth factor, as it is essential for a normal embryonic development and is highly expressed in embryonic and neonatal tissues.[30]
Variants
[edit]A splice variant of IGF-1 sharing an identical mature region, but with a different E domain is known as mechano-growth factor (MGF).[31]
Related disorders
[edit]Laron syndrome
[edit]
Laron syndrome (LS), also known as growth hormone insensitivity or growth hormone receptor deficiency (GHRD), is an autosomal recessive disorder characterized by a lack of insulin-like growth factor 1 (IGF-1; somatomedin-C) production in response to growth hormone (GH; hGH; somatotropin).[32] It is usually caused by inherited growth hormone receptor (GHR) mutations.[33][32]
Affected individuals classically present with short stature between −4 and −10 standard deviations below median height, obesity, craniofacial abnormalities, micropenis, low blood sugar, and low serum IGF-1 despite elevated basal serum GH.[34][35][36]
LS is a very rare condition with a total of 250 known individuals worldwide.[37][35] The genetic origins of these individuals have been traced back to Mediterranean, South Asian, and Semitic ancestors, with the latter group comprising the majority of cases.[35] Molecular genetic testing for growth hormone receptor gene mutations confirms the diagnosis of LS, but clinical evaluation may include laboratory analysis of basal GH, IGF-1 and IGFBP levels, GH stimulation testing, and/or GH trial therapy.
People with LS are unresponsive to growth hormone therapy; the disease is instead treated mainly with recombinant IGF-1, Mecasermin.[38]
Evidence has suggested that people with Laron syndrome have a reduced risk of developing cancer and diabetes mellitus type II, with a significantly reduced incidence and delayed age of onset of these diseases compared to their unaffected relatives.[39][40] The molecular mechanisms of increased longevity and protection from age-related disease among people with LS is an area of active investigation.[41]Acromegaly
[edit]Acromegaly is a syndrome caused by the anterior pituitary gland producing excess growth hormone (GH).[42] A number of disorders may increase the pituitary's GH output, although most commonly it involves a tumor called pituitary adenoma, derived from a distinct type of cell (somatotrophs). It leads to anatomical changes and metabolic dysfunction caused by elevated GH and IGF-1 levels.[43]
High level of IGF-1 in acromegaly is related to an increased risk of some cancers, particularly colon cancer and thyroid cancer.[44]
Use as a diagnostic test
[edit]Growth hormone deficiency
[edit]IGF-1 levels can be analyzed and used by physicians as a screening test for growth hormone deficiency (GHD),[45] acromegaly and gigantism.[46] However, IGF-1 has been shown to be a bad diagnostic screening test for growth hormone deficiency.[47][48]
The ratio of IGF-1 and insulin-like growth factor-binding protein 3 has been shown to be a useful diagnostic test for GHD.[49][50]
Liver fibrosis
[edit]Low serum IGF-1 levels have been suggested as a biomarker for predicting fibrosis, but not steatosis, in people with metabolic dysfunction–associated steatotic liver disease.[51]
Causes of elevated IGF-1 levels
[edit]- Medical conditions:
- acromegaly (especially when GH is also high)[43]
- delayed puberty[52]
- pregnancy[53]
- hyperthyroidism[53]
- some rare tumors, such as carcinoids, secreting IGF-1[54]
- Diet:
- High-protein diet[55]
- consumption of dairy products (except for cheese)[56]
- consumption of fish[56]
- IGF-1 assay problems[53]
Calorie restriction has been found to have no effect on IGF-1 levels.[55]
Causes of reduced IGF-1 levels
[edit]- Metabolic dysfunction–associated steatotic liver disease, especially at advanced stages of steatohepatitis and fibrosis[57]
Health effects
[edit]Mortality
[edit]Both high and low levels of IGF‐1 increase mortality risk, with the mid‐range (120–160 ng/ml) being associated with the lowest mortality.[58]
Cancer
[edit]Higher levels of IGF-1 are associated with an increased risk of breast cancer, colon cancer and lung cancer.[58][59]
Dairy consumption
[edit]It has been suggested that consumption of IGF-1 in dairy products could increase cancer risk, particularly prostate cancer.[60][61] However, significant levels of intact IGF-1 from oral consumption are not absorbed as they are digested by gastric enzymes.[61][62] IGF-1 present in food is not expected to be active within the body in the way that IGF-1 is produced by the body itself.[61]
The Food and Drug Administration has stated that IGF-I concentrations in milk are not significant when evaluated against concentrations of IGF-I endogenously produced in humans.[63]
A 2018 review by the Committee on Carcinogenicity of Chemicals in Food, Consumer Products and the Environment (COC) concluded that there is "insufficient evidence to draw any firm conclusions as to whether exposure to dietary IGF-1 is associated with an increased incidence of cancer in consumers".[61] Certain dairy processes such as fermentation are known to significantly decrease IGF-1 concentrations.[64] The British Dietetic Association has described the idea that milk promotes hormone related cancerous tumor growth as a myth, stating "no link between dairy containing diets and risk of cancer or promoting cancer growth as a result of hormones".[65]
Cardiovascular disease
[edit]Increased IGF-1 levels are associated with a 16% lower risk of cardiovascular disease and a 28% reduction of cardiovascular events.[66]
Diabetes
[edit]Low IGF-1 levels are shown to increase the risk of developing type 2 diabetes and insulin resistance.[67] On the other hand, a high IGF-1 bioavailability in people with diabetes may delay or prevent diabetes-associated complications, as it improves impaired small blood vessel function.[67]
IGF-1 has been characterized as an insulin sensitizer.[68]
Low serum IGF‐1 levels can be considered an indicator of liver fibrosis in type 2 diabetes mellitus patients.[69]
See also
[edit]References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000017427 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000020053 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Tahimic CG, Wang Y, Bikle DD (2013). "Anabolic effects of IGF-1 signaling on the skeleton". Frontiers in Endocrinology. 4: 6. doi:10.3389/fendo.2013.00006. PMC 3563099. PMID 23382729.
- ^ Salmon WD, Daughaday WH (June 1957). "A hormonally controlled serum factor which stimulates sulfate incorporation by cartilage in vitro". The Journal of Laboratory and Clinical Medicine. 49 (6): 825–836. PMID 13429201.
- ^ Meuli C, Zapf J, Froesch ER (April 1978). "NSILA-carrier protein abolishes the action of nonsuppressible insulin-like activity (NSILA-S) on perfused rat heart". Diabetologia. 14 (4): 255–259. doi:10.1007/BF01219425. PMID 640301.
- ^ Höppener JW, de Pagter-Holthuizen P, Geurts van Kessel AH, Jansen M, Kittur SD, Antonarakis SE, et al. (1985). "The human gene encoding insulin-like growth factor I is located on chromosome 12". Human Genetics. 69 (2): 157–160. doi:10.1007/BF00293288. PMID 2982726. S2CID 5825276.
- ^ Jansen M, van Schaik FM, Ricker AT, Bullock B, Woods DE, Gabbay KH, et al. (1983). "Sequence of cDNA encoding human insulin-like growth factor I precursor". Nature. 306 (5943): 609–611. Bibcode:1983Natur.306..609J. doi:10.1038/306609a0. PMID 6358902. S2CID 4336584.
- ^ Rinderknecht E, Humbel RE (April 1978). "The amino acid sequence of human insulin-like growth factor I and its structural homology with proinsulin". The Journal of Biological Chemistry. 253 (8): 2769–2776. doi:10.1016/S0021-9258(17)40889-1. PMID 632300.
- ^ Callaway E (February 2022). "Big dog, little dog: mutation explains range of canine sizes". Nature. 602 (7895): 18. Bibcode:2022Natur.602...18C. doi:10.1038/d41586-022-00209-0. PMID 35087254. S2CID 246359754.
- ^ Decourtye L, Mire E, Clemessy M, Heurtier V, Ledent T, Robinson IC, et al. (2017). "IGF-1 Induces GHRH Neuronal Axon Elongation during Early Postnatal Life in Mice". PLOS ONE. 12 (1): e0170083. Bibcode:2017PLoSO..1270083D. doi:10.1371/journal.pone.0170083. PMC 5226784. PMID 28076448.
- ^ Suwa S, Katsumata N, Maesaka H, Tokuhiro E, Yokoya S (December 1988). "Serum insulin-like growth factor I (somatomedin-C) level in normal subjects from infancy to adulthood, pituitary dwarfs and normal variant short children". Endocrinologia Japonica. 35 (6): 857–864. doi:10.1507/endocrj1954.35.857. PMID 3250861. S2CID 6965802.
- ^ Landin-Wilhelmsen K, Wilhelmsen L, Lappas G, Rosén T, Lindstedt G, Lundberg PA, et al. (September 1994). "Serum insulin-like growth factor I in a random population sample of men and women: relation to age, sex, smoking habits, coffee consumption and physical activity, blood pressure and concentrations of plasma lipids, fibrinogen, parathyroid hormone and osteocalcin". Clinical Endocrinology. 41 (3): 351–357. doi:10.1111/j.1365-2265.1994.tb02556.x. PMID 7955442. S2CID 24346368.
- ^ Keating GM (2008). "Mecasermin". BioDrugs. 22 (3): 177–188. doi:10.2165/00063030-200822030-00004. PMID 18481900.
- ^ Guan J, Li F, Kang D, Anderson T, Pitcher T, Dalrymple-Alford J, et al. (January 2023). "Cyclic Glycine-Proline (cGP) Normalises Insulin-Like Growth Factor-1 (IGF-1) Function: Clinical Significance in the Ageing Brain and in Age-Related Neurological Conditions". Molecules. 28 (3): 1021. doi:10.3390/molecules28031021. PMC 9919809. PMID 36770687.
- ^ Larsson SC, Michaëlsson K, Burgess S (September 2020). "IGF-1 and cardiometabolic diseases: a Mendelian randomisation study". Diabetologia. 63 (9): 1775–1782. doi:10.1007/s00125-020-05190-9. PMC 7406523. PMID 32548700.
- ^ a b Guo J, Xie J, Zhou B, Găman MA, Kord-Varkaneh H, Clark CC, et al. (1 April 2020). "The influence of zinc supplementation on IGF-1 levels in humans: A systematic review and meta-analysis". Journal of King Saud University - Science. 32 (3): 1824–1830. doi:10.1016/j.jksus.2020.01.018. ISSN 1018-3647.
- ^ Xie W, Tang Z, Guo Y, Zhang C, Zhang H, Han Y, et al. (September 2019). "Seasonal expressions of growth hormone receptor, insulin-like growth factor 1 and insulin-like growth factor 1 receptor in the scented glands of the muskrats (Ondatra zibethicus)". General and Comparative Endocrinology. 281: 58–66. doi:10.1016/j.ygcen.2019.05.014. PMID 31121166. S2CID 163168020.
- ^ Levine ME, Suarez JA, Brandhorst S, Balasubramanian P, Cheng CW, Madia F, et al. (March 2014). "Low protein intake is associated with a major reduction in IGF-1, cancer, and overall mortality in the 65 and younger but not older population". Cell Metabolism. 19 (3): 407–417. doi:10.1016/j.cmet.2014.02.006. PMC 3988204. PMID 24606898.
- ^ Yakar S, Rosen CJ, Beamer WG, Ackert-Bicknell CL, Wu Y, Liu JL, et al. (September 2002). "Circulating levels of IGF-1 directly regulate bone growth and density". The Journal of Clinical Investigation. 110 (6): 771–781. doi:10.1172/JCI15463. PMC 151128. PMID 12235108.
- ^ Peruzzi F, Prisco M, Dews M, Salomoni P, Grassilli E, Romano G, et al. (October 1999). "Multiple signaling pathways of the insulin-like growth factor 1 receptor in protection from apoptosis". Molecular and Cellular Biology. 19 (10): 7203–7215. doi:10.1128/mcb.19.10.7203. PMC 84713. PMID 10490655.
- ^ Juin P, Hueber AO, Littlewood T, Evan G (June 1999). "c-Myc-induced sensitization to apoptosis is mediated through cytochrome c release". Genes & Development. 13 (11): 1367–1381. doi:10.1101/gad.13.11.1367. PMC 316765. PMID 10364155.
- ^ Moloney AM, Griffin RJ, Timmons S, O'Connor R, Ravid R, O'Neill C (February 2010). "Defects in IGF-1 receptor, insulin receptor and IRS-1/2 in Alzheimer's disease indicate possible resistance to IGF-1 and insulin signalling". Neurobiology of Aging. 31 (2): 224–243. doi:10.1016/j.neurobiolaging.2008.04.002. PMID 18479783. S2CID 14265087.
- ^ a b c Clemmons DR (June 2012). "Metabolic actions of insulin-like growth factor-I in normal physiology and diabetes". Endocrinology and Metabolism Clinics of North America. 41 (2): 425–43, vii–viii. doi:10.1016/j.ecl.2012.04.017. PMC 3374394. PMID 22682639.
- ^ a b Bikle DD, Tahimic C, Chang W, Wang Y, Philippou A, Barton ER (November 2015). "Role of IGF-I signaling in muscle bone interactions". Bone. 80: 79–88. doi:10.1016/j.bone.2015.04.036. PMC 4600536. PMID 26453498.
- ^ Clemmons DR (January 2004). "The relative roles of growth hormone and IGF-1 in controlling insulin sensitivity". The Journal of Clinical Investigation. 113 (1): 25–27. doi:10.1172/JCI200420660. PMC 300772. PMID 14702105.
- ^ a b García-Mato Á, Cervantes B, Murillo-Cuesta S, Rodríguez-de la Rosa L, Varela-Nieto I (September 2021). "Insulin-like Growth Factor 1 Signaling in Mammalian Hearing". Genes. 12 (10): 1553. doi:10.3390/genes12101553. PMC 8535591. PMID 34680948.
- ^ Annunziata M, Granata R, Ghigo E (March 2011). "The IGF system". Acta Diabetologica. 48 (1): 1–9. doi:10.1007/s00592-010-0227-z. PMID 21042815. S2CID 24843614.
- ^ Winston BW, Ni A, Aurora RC (2006). "Insulin-like Growth Factors". In Laurent GJ, Shapiro SD (eds.). Encyclopedia of Respiratory Medicine. pp. 339–346. doi:10.1016/B0-12-370879-6/00453-1. ISBN 978-0-12-370879-3.
GF-II appears to be essential for normal embryonic development and, as such, IGF-II is thought to be a fetal growth factor. IGF-II is highly expressed in embryonic and neonatal tissues and promotes proliferation of many cell types primarily of fetal origin.
- ^ Carpenter V, Matthews K, Devlin G, Stuart S, Jensen J, Conaglen J, et al. (February 2008). "Mechano-growth factor reduces loss of cardiac function in acute myocardial infarction". Heart, Lung & Circulation. 17 (1): 33–39. doi:10.1016/j.hlc.2007.04.013. PMID 17581790.
- ^ a b Laron Z (2004). "Laron Syndrome (Primary Growth Hormone Resistance or Insensitivity): The Personal Experience 1958–2003". The Journal of Clinical Endocrinology & Metabolism. 89 (3): 1031–1044. doi:10.1210/jc.2003-031033. ISSN 0021-972X. PMID 15001582.
- ^ Hamosh A, O'Neill M, Phillips J, McKusick V. "# 262500 LARON SYNDROME". omim.org. McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University School of Medicine. Retrieved 10 November 2020.
- ^ Laron Z, Ginsberg S, Lilos P, Arbiv M, Vaisman N (2006). "Body composition in untreated adult patients with Laron syndrome (primary GH insensitivity)". Clin. Endocrinol. 65 (1): 114–7. doi:10.1111/j.1365-2265.2006.02558.x. PMID 16817829. S2CID 11524548.
- ^ a b c Rosenbloom AL (13 November 2019). "Growth Hormone Resistance". Medscape Reference. Retrieved 3 November 2020.
- ^ Murray PG, Clayton PE (16 November 2016). Disorders of Growth Hormone in Childhood. MDText.com, Inc. PMID 25905205. Retrieved 3 November 2020.
- ^ Leger J. "ORPHA:633". orpha.net. Retrieved 30 October 2020.
- ^ Grimberg A, DiVall SA, Polychronakos C (2016). "Guidelines for Growth Hormone and Insulin-Like Growth Factor-I Treatment in Children and Adolescents: Growth Hormone Deficiency, Idiopathic Short Stature, and Primary Insulin-Like Growth Factor-I Deficiency". Hormone Research in Paediatrics. 86 (6): 361–397. doi:10.1159/000452150. PMID 27884013. S2CID 5798925.
- ^ Laron Z, Kopchick J (25 November 2010). Laron Syndrome - From Man to Mouse: Lessons from Clinical and Experimental Experience. Springer Science & Business Media. pp. 339, 341. ISBN 978-3-642-11183-9.
- ^ Laron Z, Kauli R, Lapkina L, Werner H (2017). "IGF-I deficiency, longevity and cancer protection of patients with Laron syndrome". Reviews in Mutation Research. 772 (123–133): 123–133. doi:10.1016/j.mrrev.2016.08.002. PMID 28528685.
- ^ Werner H, Lapkina-Gendler L, Laron Z (2017). "Fifty years on: New lessons from the laron syndrome". Israel Medical Association Journal. 19 (1): 6–7. PMID 28457105.
- ^ "Acromegaly - NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 11 May 2024.
- ^ a b Giustina A, Chanson P, Kleinberg D, Bronstein MD, Clemmons DR, Klibanski A, et al. (April 2014). "Expert consensus document: A consensus on the medical treatment of acromegaly". Nature Reviews. Endocrinology. 10 (4): 243–248. doi:10.1038/nrendo.2014.21. PMID 24566817.
- ^ AlDallal S (August 2018). "Acromegaly: a challenging condition to diagnose". review. International Journal of General Medicine. 11: 337–343. doi:10.2147/IJGM.S169611. PMC 6112775. PMID 30197531.
- ^ Shen Y, Zhang J, Zhao Y, Yan Y, Liu Y, Cai J (April 2015). "Diagnostic value of serum IGF-1 and IGFBP-3 in growth hormone deficiency: a systematic review with meta-analysis". European Journal of Pediatrics. 174 (4): 419–427. doi:10.1007/s00431-014-2406-3. PMID 25213432.
- ^ Trivellin G, Daly AF, Faucz FR, Yuan B, Rostomyan L, Larco DO, et al. (December 2014). "Gigantism and acromegaly due to Xq26 microduplications and GPR101 mutation". The New England Journal of Medicine. 371 (25): 2363–2374. doi:10.1056/NEJMoa1408028. PMC 4291174. PMID 25470569.
- ^ Iwayama H, Kitagawa S, Sada J, Miyamoto R, Hayakawa T, Kuroyanagi Y, et al. (August 2021). "Insulin-like growth factor-1 level is a poor diagnostic indicator of growth hormone deficiency". Scientific Reports. 11 (1): 16159. Bibcode:2021NatSR..1116159I. doi:10.1038/s41598-021-95632-0. PMC 8352887. PMID 34373538.
- ^ Fatani TH (February 2023). "Diagnostic Value of IGF-1 in Growth Hormone-Deficient Children: Is a Second Growth Hormone Stimulation Test Necessary?". Journal of the Endocrine Society. 7 (4): bvad018. doi:10.1210/jendso/bvad018. PMC 9954969. PMID 36846213.
- ^ Haj-Ahmad LM, Mahmoud MM, Sweis NW, Bsisu I, Alghrabli AM, Ibrahim AM, et al. (March 2023). "Serum IGF-1 to IGFBP-3 Molar Ratio: A Promising Diagnostic Tool for Growth Hormone Deficiency in Children". The Journal of Clinical Endocrinology and Metabolism. 108 (4): 986–994. doi:10.1210/clinem/dgac609. PMID 36251796.
- ^ Lambrecht N (March 2023). "IGF-1/IGFBP-3 Serum Ratio as a Robust Measure to Determine GH Deficiency and Guide Human Recombinant GH Therapy". The Journal of Clinical Endocrinology and Metabolism. 108 (4): e54–e55. doi:10.1210/clinem/dgac687. PMID 36454697.
- ^ Marques V, Afonso MB, Bierig N, Duarte-Ramos F, Santos-Laso Á, Jimenez-Agüero R, et al. (23 June 2021). "Adiponectin, Leptin, and IGF-1 Are Useful Diagnostic and Stratification Biomarkers of NAFLD". Frontiers in Medicine. 8: 683250. doi:10.3389/fmed.2021.683250. PMC 8260936. PMID 34249975.
- ^ Imran SA, Pelkey M, Clarke DB, Clayton D, Trainer P, Ezzat S (2010). "Spuriously Elevated Serum IGF-1 in Adult Individuals with Delayed Puberty: A Diagnostic Pitfall". primary. International Journal of Endocrinology. 2010: 1–4. doi:10.1155/2010/370692. PMC 2939391. PMID 20862389.
- ^ a b c Freda PU (August 2009). "Monitoring of acromegaly: what should be performed when GH and IGF-1 levels are discrepant?". review. Clinical Endocrinology. 71 (2): 166–170. doi:10.1111/j.1365-2265.2009.03556.x. PMC 3654652. PMID 19226264.
- ^ Phillips JD, Yeldandi A, Blum M, de Hoyos A (October 2009). "Bronchial carcinoid secreting insulin-like growth factor-1 with acromegalic features". primary. The Annals of Thoracic Surgery. 88 (4): 1350–1352. doi:10.1016/j.athoracsur.2009.02.042. PMID 19766843.
- ^ a b Kazemi A, Speakman JR, Soltani S, Djafarian K (June 2020). "Effect of calorie restriction or protein intake on circulating levels of insulin like growth factor I in humans: A systematic review and meta-analysis". Clinical Nutrition. 39 (6): 1705–1716. doi:10.1016/j.clnu.2019.07.030. PMID 31431306.
- ^ a b Watling CZ, Kelly RK, Tong TYN, Piernas C, Watts EL, Tin Tin S, Knuppel A, Schmidt JA, Travis RC, Key TJ, Perez-Cornago A. (2023). "Associations between food group intakes and circulating insulin-like growth factor-I in the UK Biobank: a cross-sectional analysis". European Journal of Nutrition. 62 (1): 115–124. doi:10.1007/s00394-022-02954-4. PMC 9899744. PMID 35906357.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ma IL, Stanley TL (July 2023). "Growth hormone and nonalcoholic fatty liver disease". Immunometabolism. 5 (3): e00030. doi:10.1097/IN9.0000000000000030. PMC 10373851. PMID 37520312.
- ^ a b Rahmani J, Montesanto A, Giovannucci E, Zand H, Barati M, Kopchick JJ, et al. (February 2022). "Association between IGF-1 levels ranges and all-cause mortality: A meta-analysis". Aging Cell. 21 (2): e13540. doi:10.1111/acel.13540. PMC 8844108. PMID 35048526.
- ^ Murphy N, Knuppel A, Papadimitriou N, Martin RM, Tsilidis KK, Smith-Byrne K, et al. (2020). "Insulin-like growth factor-1, insulin-like growth factor-binding protein-3, and breast cancer risk: observational and Mendelian randomization analyses with ∼430 000 women". Annals of Oncology. 31 (5): 641–649. doi:10.1016/j.annonc.2020.01.066. PMC 7221341. PMID 32169310.
- ^ Harrison S, Lennon R, Holly J, Higgins JP, Gardner M, Perks C, et al. (June 2017). "Does milk intake promote prostate cancer initiation or progression via effects on insulin-like growth factors (IGFs)? A systematic review and meta-analysis". Cancer Causes & Control. 28 (6): 497–528. doi:10.1007/s10552-017-0883-1. PMC 5400803. PMID 28361446.
- ^ a b c d "Statement on possible carcinogenic hazard to consumers from insulin-like growth factor-1 (IGF-1) in the diet" (PDF). assets.publishing.service.gov.uk. Retrieved 4 February 2023.
- ^ Juskevich JC, Guyer CG (August 1990). "Bovine Growth Hormone: Human Food Safety Evaluation". Science. 249 (4971): 875–84. doi:10.1126/science.2203142. JSTOR 2877952. PMID 2203142.
- ^ "FDA rejects petition to ban rBST". American Veterinary Medical Association. 2000. Archived from the original on 13 August 2020.
- ^ Meyer Z, Höflich C, Wirthgen E, Olm S, Hammon HM, Hoeflich A (August 2017). "Analysis of the IGF-system in milk from farm animals - Occurrence, regulation, and biomarker potential". Growth Hormone & IGF Research. 35: 1–7. doi:10.1016/j.ghir.2017.05.004. PMID 28544872.
- ^ "Cancer Diets: Myths and More". British Dietetic Association. 2024. Archived from the original on 26 July 2024.
- ^ Li T, Zhao Y, Yang X, Feng Y, Li Y, Wu Y, et al. (December 2022). "Association between insulin-like growth factor-1 and cardiovascular events: a systematic review and dose-response meta-analysis of cohort studies". Journal of Endocrinological Investigation. 45 (12): 2221–2231. doi:10.1007/s40618-022-01819-1. PMID 35596917. S2CID 248924624.
- ^ a b Biadgo B, Tamir W, Ambachew S (1 May 2021). "Insulin-like Growth Factor and its Therapeutic Potential for Diabetes Complications - Mechanisms and Metabolic Links: A Review". The Review of Diabetic Studies. 16 (1): 24–34. doi:10.1900/RDS.2020.16.24 (inactive 1 November 2024). PMC 9380093. PMID 33905470.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ Yuen KC, Dunger DB (January 2007). "Therapeutic aspects of growth hormone and insulin-like growth factor-I treatment on visceral fat and insulin sensitivity in adults". Diabetes, Obesity & Metabolism. 9 (1): 11–22. doi:10.1111/j.1463-1326.2006.00591.x. PMID 17199714.
- ^ Miyauchi S, Miyake T, Miyazaki M, Eguchi T, Niiya T, Yamamoto S, et al. (July 2019). "Insulin-like growth factor-1 is inversely associated with liver fibrotic markers in patients with type 2 diabetes mellitus". Journal of Diabetes Investigation. 10 (4): 1083–1091. doi:10.1111/jdi.13000. PMC 6626962. PMID 30592792.
External links
[edit]- Insulin-Like+Growth+Factor+I at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: P05019 (Insulin-like growth factor I) at the PDBe-KB.


















![3lri: Solution structure and backbone dynamics of long-[Arg(3)]insulin-like growth factor-I](http://upload.wikimedia.org/wikipedia/commons/thumb/3/3b/PDB_3lri_EBI.jpg/180px-PDB_3lri_EBI.jpg)